Implications
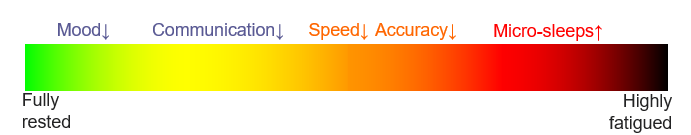
Along with emotional intelligence and cognitive skills, fatigue also takes a toll on mood, motivation and productivity; reducing an individuals willingness to ‘go the extra mile’. Fatigue impairments can lead to misunderstandings, miscommunication, escalated encounters, longer resolution times and service errors, resulting in dissatisfied customers, adverse outcomes and complaints. Furthermore, fatigue can ripple through organisations, leading to absenteeism and higher staff turnover, further diminishing quality of service delivery.
Mitigating Fatigue for Enhanced Service Delivery
Organisations in service-oriented sectors can enhance service quality by prioritising fatigue management strategies. Investing in employee well-being by promoting healthy sleep practices, managing workloads, and providing opportunities for rejuvenation can have a profound impact. Encouraging short breaks, facilitating better work-life balance, and fostering a supportive work culture can significantly reduce the prevalence of fatigue.
References
Gordon, A. M., & Chen, S. (2014). The Role of Sleep in Interpersonal Conflict: Do Sleepless Nights Mean Worse Fights? Social Psychological and Personality Science, 5(2), 168–175. https://doi.org/10.1177/1948550613488952
Killgore, W., Kahn-Greene, E., Lipizzi, E., Newman, R., Kamimori, G. & Balkin, T. (2008). Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep medicine. 9. 517-26. https://doi.org/10.1016/j.sleep.2007.07.003
Paterson, J.L., Dorrian, J., Ferguson,S.A., Jay, S.M., Lamond, N., Murphy, P.J., Campbell, S.S., & Dawson, D.
(2011) Changes in structural aspects of mood during 39–66h of sleep loss using matched controls,
Applied Ergonomics, 42(2), 196-201, https://doi.org/10.1016/j.apergo.2010.06.014.
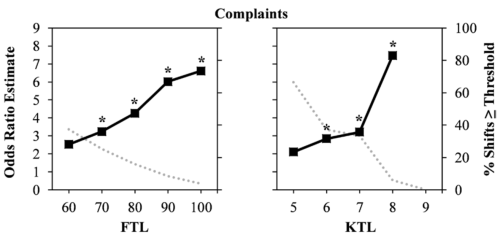
Riedy, S. M., Dawson, D. & Vila, B. (2019). U.S. police rosters: Fatigue and public complaints, Sleep, 42(3), zsy231, https://doi.org/10.1093/sleep/zsy231
Riedy, S., Dawson, D., Fekedulegn, D., Andrew, M., Vila, B., and Violanti, J. (2020), Fatigue and Short-term Unplanned Absences Among Police Officers, Policing: an International Journal, http://doi.org/10.1108/PIJPSM-10-2019-0165
Whitney, P., Hinson, J., Jackson, M. & Van Dongen, H. (2015) Feedback Blunting: Total Sleep Deprivation Impairs Decision Making that Requires Updating Based on Feedback, Sleep, 38(5), 745–754. https://doi.org/10.5665/sleep.4668





 What’s the point?
What’s the point?